Visit us: Mon - Fri: 9:00 - 18:30
Braley Care Homes 6192 US 60 Hurricane, WV 25526
Alzheimer’s Care in Huntington West Virginia
What is Alzheimer’s?
Alzheimer's disease is the most common type of dementia. It is a progressive disease beginning with mild memory loss and possibly leading to loss of the ability to carry on a conversation and respond to the environment. Alzheimer's disease involves parts of the brain that control thought, memory, and language.
What Triggers Alzheimer’s?
Scientists don’t yet fully understand what causes Alzheimer’s disease in most people. The causes probably include a combination of age-related changes in the brain, along with genetic, environmental, and lifestyle factors. The importance of any one of these factors in increasing or decreasing the risk of Alzheimer’s disease may differ from person to person. Alzheimer’s disease is a progressive brain disease. It is characterized by changes in the brain—including amyloid plaques and neurofibrillary, or tau, tangles—that result in loss of neurons and their connections. These and other changes affect a person’s ability to remember and think and, eventually, to live independently
What is Alzheimer’s?
Alzheimer's disease is the most common type of dementia. It is a progressive disease beginning with mild memory loss and possibly leading to loss of the ability to carry on a conversation and respond to the environment. Alzheimer's disease involves parts of the brain that control thought, memory, and language.
What Triggers Alzheimer’s?
Scientists don’t yet fully understand what causes Alzheimer’s disease in most people. The causes probably include a combination of age-related changes in the brain, along with genetic, environmental, and lifestyle factors. The importance of any one of these factors in increasing or decreasing the risk of Alzheimer’s disease may differ from person to person.
Alzheimer’s disease is a progressive brain disease. It is characterized by
changes in the brain—including amyloid plaques and neurofibrillary, or tau, tangles—that result in loss of neurons and their connections. These and other changes affect a person’s ability to remember and think and, eventually, to live independently.
Causes and Risk Factors for Alzheimer's Disease
Alzheimer's disease is an intricate puzzle with many pieces - genetics, lifestyle, and environment only being a few of them. Though some risks like age or family history can't be avoided, today researchers are discovering more controllable factors that could help reduce its risk! Keeping one’s mind sharp has never been so important
(and possible)!

Other risk factors

Family history

Age
The greatest known risk factor for Alzheimer’s and other dementias is increasing age, but these disorders are not a normal part of aging. While age increases risk, it is not a direct cause of Alzheimer’s.
Most individuals with the disease are 65 and older. After age 65, the risk of Alzheimer’s doubles every five years. After age 85, the risk reaches nearly one-third.
Another strong risk factor is family history. Those who have a parent, brother or sister with Alzheimer’s are more likely to develop the disease. The risk increases if more than one family member has the illness. When diseases tend to run in families, either heredity (genetics), environmental factors, or both, may play a role.
Scientists know genes are involved in Alzheimer’s. Two categories of genes influence whether a person develops a disease: risk genes and deterministic genes. Alzheimer’s genes have been found in both categories. It is estimated that less than 1% of Alzheimer’s cases are caused by deterministic genes (genes that cause a disease, rather than increase the risk of developing a disease).
While age, family history and heredity are all risk factors we can’t change, research is beginning to reveal clues about other risk factors we may be able to influence through general lifestyle and wellnesschoices and effective management of other health conditions.
What are the stages of Alzheimer's
You can help support your loved one with Alzheimer’s by learning more about how the condition unfolds.
The stages don’t always fall into neat boxes, and the symptoms might vary — but they can be a guide and help you plan for your friend or relative’s care.
Stage 1: No Impairment
During this stage, Alzheimer’s is not detectable and no memory problems or other symptoms of dementia are evident.
Stage 2: Very Mild Decline
The senior may notice minor memory problems or lose things around the house, although not to the point where the memory loss can easily be distinguished from normal age-related memory loss. The person will still do well on memory tests and the disease is unlikely to be detected by loved ones or physicians.
Stage 3: Mild Decline
At this stage, the family members and friends of the senior may begin to notice cognitive problems. Performance on memory tests are affected and physicians will be able to detect impaired cognitive function.
People in stage 3 will have difficulty in many areas including:
• Finding the right word during conversations
• Organizing and planning
• Remembering names of new acquaintances
People with stage three Alzheimer’s may also frequently lose personal possessions, including valuables.
Stage 4 : Moderate Decline
In stage four of Alzheimer’s, clear-cut symptoms of the disease are apparent. People with stage four of Alzheimer’s:
• Have difficulty with simple arithmetic
• Have poor short-term memory (may not recall what they ate for breakfast, for example)
• Inability to manage finance and pay bills
• May forget details about their life histories
Stage 5: Moderately Severe Decline
During the fifth stage of Alzheimer’s, people begin to need help with many day-to-day activities. People in stage five of the disease may experience:
• Difficulty dressing appropriately
• Inability to recall simple details about themselves such as their own phone number
• Significant confusion
On the other hand, people in stage five maintain functionality. They typically can still bathe and toilet independently. They also usually still know their family members and some detail about their personal histories, especially their childhood and youth.
Stage 6: Severe Decline
People with the sixth stage of Alzheimer’s need constant supervision and frequently require professional care. Symptoms include:
• Confusion or unawareness of environment and surroundings
• Inability to recognize faces except for the closest friends and relatives
• Inability to remember most details of personal history
• Loss of bladder and bowel control
• Major personality changes and potential behavior problems
• The need for assistance with activities of daily living such as toileting and bathing
• Wandering
Stages 7: Very Severe Decline
Stage seven is the final stage of Alzheimer’s. Because the disease is a terminal illness, people in stage seven are nearing death. In stage seven of the disease, people lose the ability to communicate or respond to their environment. While they may still be able to utter words and phrases, they have no insight into their condition and need
assistance with all activities of daily living. In the final stages of Alzheimer’s, people may lose their ability to swallow.
Source: alzheimers.net
How can I help someone with Alzheimer's
When you’re a caregiver for a person with Alzheimer’s disease , one of your main goals is to help your loved one do as much they can on their own. This helps them keep their sense of independence. Break down tasks into small steps, or even write out easy-to-follow directions. (webmd.com)
Make it easier for them to dress on their own. Lay out their clothes in the order they put them on, or hand them one piece of clothing at a time. (webmd.com)
If they want to wear the same clothes every day, don’t fight it. Buy 3 or 4 sets of them.
Make sure they have loose clothes that are easy to put on. Shorts and pants with elastic waistbands and slip-on shoes are good. Skip shoelaces, buttons, and buckles. (webmd.com)
“Many communities have flowing floor plans, so residents don’t feel like they’re pacing back and forth,” says Gewirtz. “These designs can help residents be redirected easier. They’re also more intimate and not as overwhelming.”
To help residents enjoy the outdoors safely, some memory care communities have interior courtyards.
Helping with chores can boost self-esteem. Ask them to dust, sweep, fix things, sort socks, fold laundry, read a recipe for you, or measure when you cook.
Stay active. Take a walk together every day to keep muscles strong, boost mood, and help with sleep. If they can’t get around well, they may be able to use a stationary bike or resistance bands. (webmd.com)
Playing word games, doing puzzles, talking about current events, or gardening can fuel thinking and memory. Listening to music (and playing “name that tune”) can also bring back fond thoughts. Be sensitive — if you sense they feel frustrated or upset by an activity, try something else.
If an activity isn’t working, it might just be the wrong time. Try it again later.
The outcome of chores or games doesn’t matter. The time you spend together and the activities that give joy or meaning to your loved one’s day do. (webmd.com)

How can I talk to with Alzheimer's
Communicating with a person with memory loss can be difficult, but the right strategies can bridge the gap and foster a more fulfilling relationship between you and your patient or loved one.
Those struggling to communicate with a person
who has memory loss are not alone. As many as four million people in the US may have Alzheimer’s , and, as our population ages, that number is expected to increase. Anyone who is a senior caregiver is likely to be affected and will need to understand how to cope with what is happening.
Memory loss associated with aging, dementia, and Alzheimer’s typically doesn’t happen overnight. Slowly, little-by-little, it sneaks up, until one day, family members realize that they can no longer communicate in the same way with the person they’ve known for years. They suddenly can’t rely on their words and their sentences don’t match the situation.
Because we cannot see the disease—the way we see a broken arm—it’s even more confusing when caregivers see how their patient and/or loved one will have good and bad days. The days when they’re alert and clear-headed make a caregiver hopeful. Then the bad days come, and family members and caregivers feel the pain of losing their patient and/or loved one all over again. This slow and normal progression of the disease makes communication a major challenge for caregivers.
The steps described provide an excellent framework to use on your visits as you approach and converse with someone with Alzheimer’s or other dementia, and are especially relevant during the middle stages of the disease.
• Approach from the front – do not startle them.
• Establish eye contact – this shows interest in them.
• Call the person by name – again, showing interest in them.
• Get down to eye level if needed – this puts you on the same level with them.
• Let them initiate touch – they will come to you when ready.
• Give directions one step at a time – this helps keep it simple, especially for those having difficulty with processing.
Causes and Risk Factors for Alzheimer's Disease
Alzheimer's disease is an intricate puzzle with many pieces - genetics, lifestyle, and environment only being a few of them. Though some risks like age or family history can't be avoided, today researchers are discovering more controllable factors that could help reduce its risk! Keeping one’s mind sharp has never been so important
(and possible)!

Other risk factors

Family history

Age
What are the stages of Alzheimer's
You can help support your loved one with Alzheimer’s by learning more about how the condition unfolds.
The stages don’t always fall into neat boxes, and the symptoms might vary — but they can be a guide and help you plan for your friend or relative’s care.
Stage 1: No Impairment
You can help support your loved one with Alzheimer’s by learning more about how the condition unfolds.
The stages don’t always fall into neat boxes, and the symptoms might vary — but they can be a guide and help you plan for your friend or relative’s care.
Stage 2: Very Mild Decline
The senior may notice minor memory problems or lose things around the house, although not to the point where the memory loss can easily be distinguished from normal age-related memory loss. The person will still do well on memory tests and the disease is unlikely to be detected by loved ones or physicians.
Stage 3: Mild Decline
At this stage, the family members and friends of the senior may begin to notice cognitive problems. Performance on memory tests are affected and physicians will be able to detect impaired cognitive function.
People in stage 3 will have difficulty in many areas including:
• Finding the right word during conversations
• Organizing and planning
• Remembering names of new acquaintances
People with stage three Alzheimer’s may also frequently lose personal possessions, including valuables.
Stage 4: Moderate Decline
In stage four of Alzheimer’s, clear-cut symptoms of the disease are apparent. People with stage four of Alzheimer’s:
• Have difficulty with simple arithmetic
• Have poor short-term memory (may not recall what they ate for breakfast, for example)
• Inability to manage finance and pay bills
• May forget details about their life histories
Stage 5: Moderately Severe Decline
During the fifth stage of Alzheimer’s, people begin to need help with many day-to-day activities. People in stage five of the disease may experience:
• Difficulty dressing appropriately
• Inability to recall simple details about themselves such as their own phone number
• Significant confusion
On the other hand, people in stage five maintain functionality. They typically can still bathe and toilet independently. They also usually still know their family members and some detail about their personal histories, especially their childhood and youth.
Stage 6: Moderately Severe Decline
People with the sixth stage of Alzheimer’s need constant supervision and frequently require professional care. Symptoms include:
• Confusion or unawareness of environment and surroundings
• Inability to recognize faces except for the closest friends and relatives
• Inability to remember most details of personal history
• Loss of bladder and bowel control
• Major personality changes and potential behavior problems
• The need for assistance with activities of daily living such as toileting and bathing
• Wandering
Stage 7: Very Severe Decline
Stage seven is the final stage of Alzheimer’s. Because the disease is a terminal illness, people in stage seven are nearing death. In stage seven of the disease, people lose the ability to communicate or respond to their environment. While they may still be able to utter words and phrases, they have no insight into their condition and need
assistance with all activities of daily living. In the final stages of Alzheimer’s, people may lose their ability to swallow.
Source: alzheimers.net
How can I help someone with Alzheimer's
When you’re a caregiver for a person with Alzheimer’s disease , one of your main goals is to help your loved one do as much they can on their own. This helps them keep their sense of independence. Break down tasks into small steps, or even write out easy-to-follow directions. (webmd.com)
Make it easier for them to dress on their own. Lay out their clothes in the order they put them on, or hand them one piece of clothing at a time. (webmd.com)
If they want to wear the same clothes every day, don’t fight it. Buy 3 or 4 sets of them.
Make sure they have loose clothes that are easy to put on. Shorts and pants with elastic waistbands and slip-on shoes are good. Skip shoelaces, buttons, and buckles. (webmd.com)
“Many communities have flowing floor plans, so residents don’t feel like they’re pacing back and forth,” says Gewirtz. “These designs can help residents be redirected easier. They’re also more intimate and not as overwhelming.”
To help residents enjoy the outdoors safely, some memory care communities have interior courtyards.
Helping with chores can boost self-esteem. Ask them to dust, sweep, fix things, sort socks, fold laundry, read a recipe for you, or measure when you cook.
Stay active. Take a walk together every day to keep muscles strong, boost mood, and help with sleep. If they can’t get around well, they may be able to use a stationary bike or resistance bands. (webmd.com)
Playing word games, doing puzzles, talking about current events, or gardening can fuel thinking and memory. Listening to music (and playing “name that tune”) can also bring back fond thoughts. Be sensitive — if you sense they feel frustrated or upset by an activity, try something else.
If an activity isn’t working, it might just be the wrong time. Try it again later.
The outcome of chores or games doesn’t matter. The time you spend together and the activities that give joy or meaning to your loved one’s day do. (webmd.com)
How can I talk to someone with Alzheimer's
Communicating with a person with memory loss can be difficult, but the right strategies can bridge the gap and foster a more fulfilling relationship between you and your patient or loved one.
Those struggling to communicate with a person
who has memory loss are not alone. As many as four million people in the US may have Alzheimer’s , and, as our population ages, that number is expected to increase. Anyone who is a senior caregiver is likely to be affected and will need to understand how to cope with what is happening.
Memory loss associated with aging, dementia, and Alzheimer’s typically doesn’t happen overnight. Slowly, little-by-little, it sneaks up, until one day, family members realize that they can no longer communicate in the same way with the person they’ve known for years. They suddenly can’t rely on their words and their sentences don’t match the situation.
Because we cannot see the disease—the way we see a broken arm—it’s even more confusing when caregivers see how their patient and/or loved one will have good and bad days. The days when they’re alert and clear-headed make a caregiver hopeful. Then the bad days come, and family members and caregivers feel the pain of losing their patient and/or loved one all over again. This slow and normal progression of the disease makes communication a major challenge for caregivers.
The steps described provide an excellent framework to use on your visits as you approach and converse with someone with Alzheimer’s or other dementia, and are especially relevant during the middle stages of the disease.
• Approach from the front – do not startle them.
• Establish eye contact – this shows interest in them.
• Call the person by name – again, showing interest in them.
• Get down to eye level if needed – this puts you on the same level with them.
• Let them initiate touch – they will come to you when ready.
• Give directions one step at a time – this helps keep it simple, especially for those having difficulty with processing.
Understanding Memory Care
At present, a lot of assisted living centers have memory care centers operating within their facilities. However, assisted living and memory care are very different in the services they provide.
Memory care involves a more comprehensive form of elderly care as it is solely dedicated to people living with dementia, Alzheimer’s, and any other forms of memory impairment. Memory care centers are usually easy to navigate through on the chance that a patient manages to wander off but they also have staff members round the clock to provide supervision on the probability that it actually happens.
Dementia patients in the early to intermediate stages usually spend a bit of time in assisted living institutions because they are allowed to be somewhat independent and their health and safety are catered for. The rooms they stay in are private and the staff is not available 24/7 apart from emergency care staff.
Nursing homes accommodate patients with dementia who are at the later stages of their disease when they are not able to walk, talk, or eat by themselves.
Benefits Provided by Memory Care Centers
Of all forms of senior care, memory care has grown increasingly rapid and with good reason too. Memory care services are more specific as compared to assisted living as it is better poised to offer high value to a patient dealing with Alzheimer’s or dementia. Some of these benefits include less violent episodes, increased social interactions, fewer falls or injuries, reduced visits to the emergency room, or decreased need for medications.
On top of the fact that memory care centers are responsible for keeping seniors safe and promoting their physical and mental conditions, they provide patients with care services that are structured to decrease their loss of memory. These services range from basic treatments to patient-curated services designed by industry professionals who have specialized in managing dementia.
Benefits Provided by Memory Care Centers
Of all forms of senior care, memory care has grown increasingly rapid and with good reason too. Memory care services are more specific as compared to assisted living as it is better poised to offer high value to a patient dealing with Alzheimer’s or dementia. Some of these benefits include less violent episodes, increased social interactions, fewer falls or injuries, reduced visits to the emergency room, or decreased need for medications.
On top of the fact that memory care centers are responsible for keeping seniors safe and promoting their physical and mental conditions, they provide patients with care services that are structured to decrease their loss of memory. These services range from basic treatments to patient-curated services designed by industry professionals who have specialized in managing dementia.
When You Should Consider Choosing Memory Care
There are certain activities that can reduce the development of dementia and these are services you will not usually find in a nursing home. For example, scientific study has shown that doing an outdoors walk at regular times of the day can help people struggling with dementia apart from the straightforward benefits of exercise. You’ll find that a nursing home might not be so open to that idea.
Music, which is usually found in all residential living rooms for the elderly, might not be so welcome to people with dementia. Memory care staff will have to approach and speak to a patient gently before requesting to play them any music despite the fact that it has been found to offer therapeutic benefits to people with Alzheimer’s.
Perhaps the fact that staff members at a memory care unit are better trained in caring and responding to dementia-related issues such as wandering or hostilities from the patient. The chances you’ll find staff trained specifically to help people with dementia working in a nursing home are not as high as staff members working in a memory care unit.
Every state has set in place rules stipulating how staff must be trained and experience for a certain amount of time before they are deemed qualified to engage a patient with dementia. Memory care centers give more assurance on this issue as compared to nursing homes because the staffers are better skilled at patience when communicating with patients with dementia or calming them down so they can receive to be administered medicine on the chance that they become aggressive.
Memory care centers are also designed for people with dementia. Subtle things such as brightly decorated or painted walls or allowance of natural light are therapeutic aspects for people living with dementia.
Choosing whether to make a memory care facility for an elderly loved one is a tough choice. Make sure that you consider the cost, accreditation of the facility, its location, and the services it offers.
Music, which is usually found in all residential living rooms for the elderly, might not be so welcome to people with dementia. Memory care staff will have to approach and speak to a patient gently before requesting to play them any music despite the fact that it has been found to offer therapeutic benefits to people with Alzheimer’s.
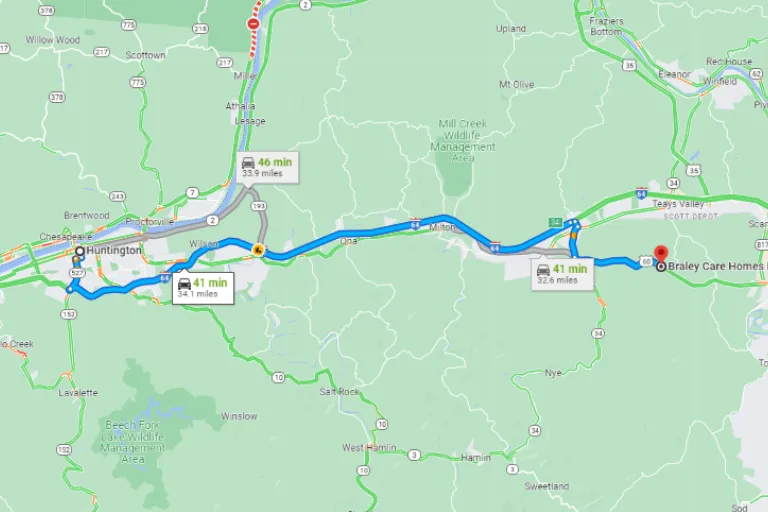
Looking for Braley Care Homes while in Huntington, WV?
When You Should Consider Choosing Memory Care
There are certain activities that can reduce the development of dementia and these are services you will not usually find in a nursing home. For example, scientific study has shown that doing an outdoors walk at regular times of the day can help people struggling with dementia apart from the straightforward benefits of exercise. You’ll find that a nursing home might not be so open to that idea.
Music, which is usually found in all residential living rooms for the elderly, might not be so welcome to people with dementia. Memory care staff will have to approach and speak to a patient gently before requesting to play them any music despite the fact that it has been found to offer therapeutic benefits to people with Alzheimer’s.
Perhaps the fact that staff members at a memory care unit are better trained in caring and responding to dementia-related issues such as wandering or hostilities from the patient. The chances you’ll find staff trained specifically to help people with dementia working in a nursing home are not as high as staff members working in a memory care unit.
Every state has set in place rules stipulating how staff must be trained and experience for a certain amount of time before they are deemed qualified to engage a patient with dementia. Memory care centers give more assurance on this issue as compared to nursing homes because the staffers are better skilled at patience when communicating with patients with dementia or calming them down so they can receive to be administered medicine on the chance that they become aggressive.
Memory care centers are also designed for people with dementia. Subtle things such as brightly decorated or painted walls or allowance of natural light are therapeutic aspects for people living with dementia.
Choosing whether to make a memory care facility for an elderly loved one is a tough choice. Make sure that you consider the cost, accreditation of the facility, its location, and the services it offers.
Music, which is usually found in all residential living rooms for the elderly, might not be so welcome to people with dementia. Memory care staff will have to approach and speak to a patient gently before requesting to play them any music despite the fact that it has been found to offer therapeutic benefits to people with Alzheimer’s.
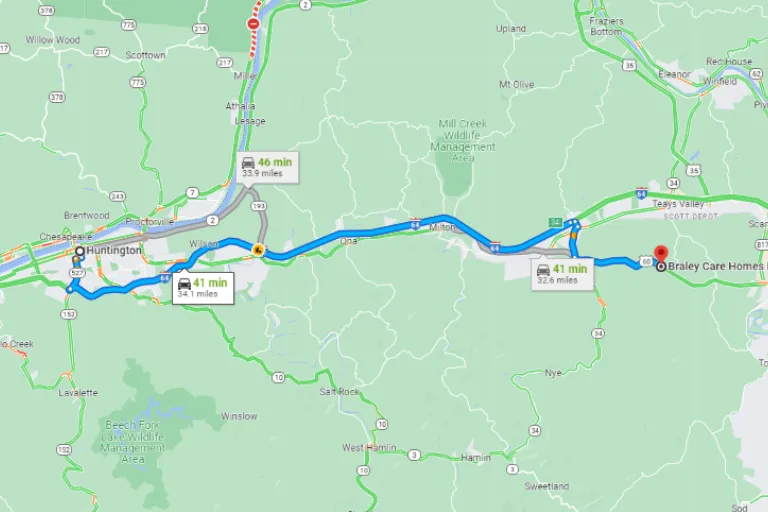
Looking for Braley Care Homes while in Charleston, WV?
Contact Us to
Schedule a Tour!
CONTACT US
Location:
Braley Care Homes
6192 US-60
Hurricane, WV 25526
Phone Numbers:
Referrals and Inquiries: (304) 767-4033
Facility Phone: (304) 201-3677
Facility Fax: (304) 201-3678
AREAS WE SERVE
BUSINESS HOURS
Monday
9:00am – 6:30pm
Tuesday
9:00am – 6:30pm
Wednesday
9:00am – 6:30pm
Thursday
9:00am – 6:30pm
Friday
9:00am – 6:30pm

Our clinic largest private mental health partnership, with a carefully selected nationwide team of Psychiatrists.
KEEP IN TOUCH.
CONTACT US
Location:
Braley Care Homes
6192 US 60
Hurricane, WV 25526
Phone Numbers:
Referrals and Inquiries: (304) 767-4033
Facility Phone: (304) 201-3677
Facility Fax: (304) 201-3678
AREAS WE SERVE
BUSINESS HOURS
Monday
9:00am – 6:30pm
Tuesday
9:00am – 6:30pm
Wednesday
9:00am – 6:30pm
Thursday
9:00am – 6:30pm
Friday
9:00am – 6:30pm



