Visit us: Mon - Fri: 9:00 - 18:30
Braley Care Homes 6192 US 60 Hurricane, WV 25526
Resources

Understanding Memory Care Costs in West Virginia: What Families Need to Know
Understanding Memory Care Costs in West Virginia: What Families Need to Know
Memory care refers to specialized long-term care services tailored to people with Alzheimer’s disease, dementia, and related cognitive impairments, combining clinical oversight with secure living environments designed to reduce wandering and maintain routines.
Families researching memory care in West Virginia need clear, actionable cost information, practical funding options, and guidance on facility selection to reduce stress and unexpected expenses. This article explains typical monthly cost ranges for memory care in West Virginia in 2025, factors that drive pricing, how memory care compares to assisted living and nursing homes, and the key public and private funding sources families can pursue. You will also find a step-by-step overview of Medicaid navigation for memory care in WV, an explanation of why memory care is often more expensive, and facility-level expectations — including how Braley Care Homes approaches transparency and assessments. Throughout the guide we use WV-focused comparisons (Hurricane, Charleston, Huntington), present EAV tables for quick reference, and include practical lists and checklists to help families act with confidence.
What Are the Average Memory Care Costs in West Virginia in 2025?
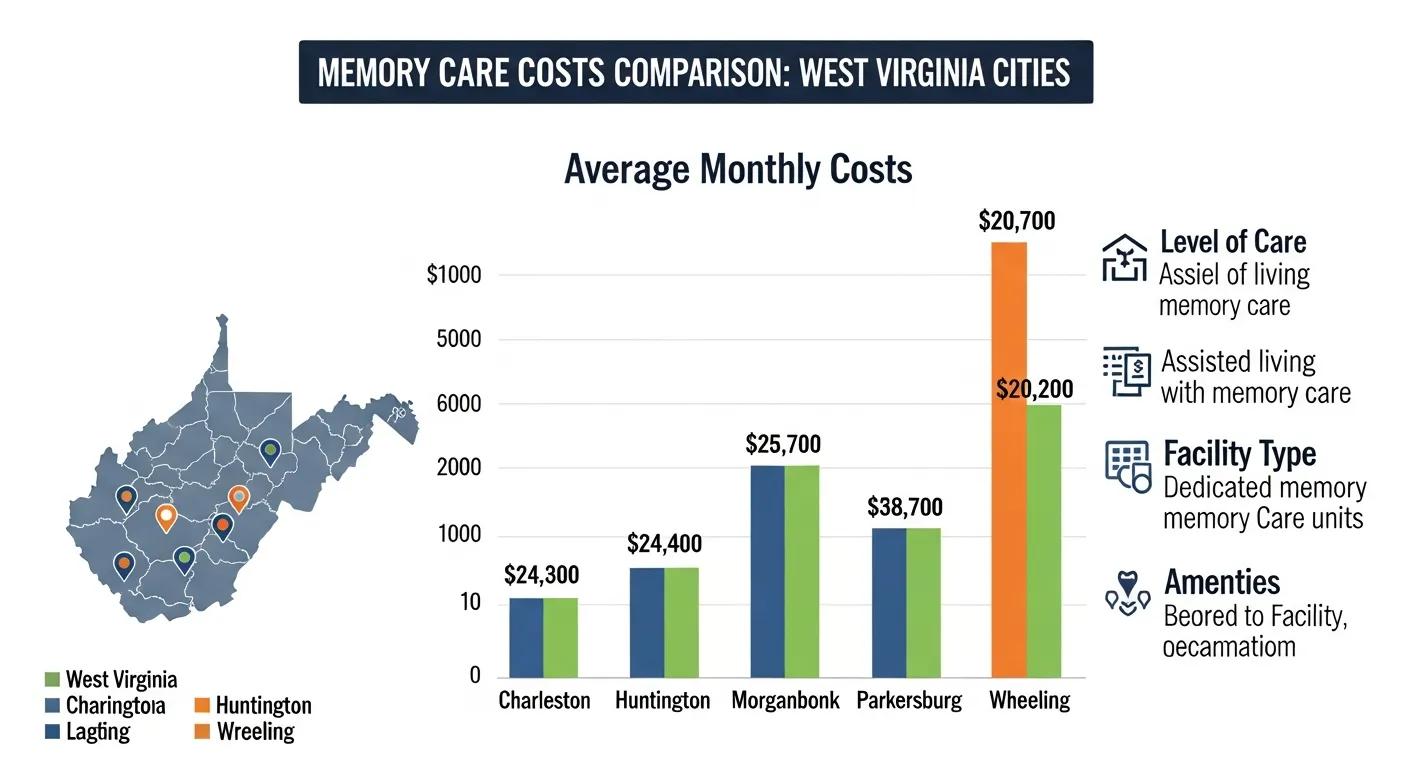
Memory care in West Virginia in 2025 typically costs more than basic assisted living because it bundles clinical oversight, secure spaces, and dementia-focused programming into a single monthly rate. Estimated statewide monthly ranges for memory care commonly fall into mid-tier and upper-tier bands driven by staffing intensity, clinical services, and facility design, and families should expect variability by city and facility type. Below we present a compact city-by-city comparison to help families benchmark local pricing and identify what drives differences between Hurricane, Charleston, and Huntington. Understanding these local ranges helps families plan budgets and focus tours on facilities that offer the right mix of safety, clinical oversight, and value.
CityTypical Monthly Memory Care Range (estimate, 2025)Common Cost DriversHurricane$3,325 – $4,643Local labor costs, availability of purpose-built facilities, proximity to metropolitan servicesCharleston$3,500 – $5,500Higher demand, larger facilities with clinical staffing, amenity packagesHuntington$3,500 – $5,500Market competition, facility age, staffing mix and training
These city-level ranges are estimates based on regional cost surveys and observed market trends for 2025; specific facility quotes will vary by resident needs and service bundles. Comparing the range across cities clarifies that location, staffing, and purpose-built design are among the largest determinants of monthly cost, which leads into more precise monthly breakdowns and examples in the next section.
How Much Does Memory Care Typically Cost per Month in WV?
Typical memory care monthly fees in West Virginia vary by level of clinical need and facility features; lower-tier properties that provide basic supervision and ADL (activities of daily living) assistance tend toward the lower end of local ranges, while purpose-built, clinically staffed communities land toward the higher end. Families should anticipate that a resident requiring moderate behavioral support and medication administration will be priced in the mid-range, whereas residents with intensive clinical needs or frequent skilled-nursing interventions will be at the top of the range. When budgeting, ask facilities to separate room & board from care-service fees and to provide sample scenarios showing how personal care needs change the monthly rate. Understanding sample billing scenarios makes it easier to see how an individual resident’s needs map to a specific price point.
What Factors Influence Memory Care Pricing in West Virginia?
Several interlocking factors determine memory care pricing: staffing ratios and specialized training, clinical oversight (RNs/LPNs/LICSW input), secure building design, programming and therapeutic activities, and local labor/rent markets. More intensive staffing and 24/7 clinical supervision increase operating costs significantly, as does purpose-built construction that includes secure wandering areas and unobstructed nurse sightlines. Facilities that invest in individualized activity programming and therapeutic services similarly charge more because those features improve quality of life and require trained personnel. Understanding which factors matter most to your loved one helps prioritize budget allocation and sharpens the questions to ask during tours.
How Do Memory Care Costs Compare Across WV Cities Like Charleston and Huntington?
Local market conditions create meaningful variations in monthly costs between Charleston, Huntington, and smaller towns like Hurricane, with demand concentration, facility supply, and local wage levels as primary drivers of variance. Urban centers typically have higher operating costs and greater demand for specialized beds, which pushes average prices upward relative to more rural markets. Differences in facility age and whether a community is purpose-built for dementia care versus adapted from assisted-living conversions also show up in price gaps. Comparing city-level ranges helps families decide whether traveling for placement or considering out-of-area options is financially and emotionally worthwhile.
How Does Memory Care Cost Compare to Assisted Living and Nursing Homes in WV?
Memory care generally costs more than standard assisted living because it includes higher staffing ratios, specialized training, and environmental safeguards, and it can be less than or comparable to skilled nursing when long-term clinical nursing care is required. Below is a concise comparison to show typical monthly differentials and included services in each care type.
Care TypeTypical Monthly Cost (estimate)Services Commonly IncludedMemory Care$3,325 – $5,50024/7 supervision, dementia programming, ADL assistance, medication administrationAssisted Living$2,000 – $4,000ADL help, basic supervision, meals, social activitiesNursing Home (long-term)$4,000 – $8,000+Skilled nursing, medical rehab, higher clinical oversight
This comparison highlights that memory care sits between assisted living and full nursing care in price and service scope because it targets cognitive impairment specifically while preserving a residential, activity-focused environment. Knowing these distinctions helps families choose a setting that balances safety and cost for the resident’s clinical profile.
What Financial Assistance Options Are Available for Memory Care in West Virginia?

Families can pursue several funding sources to offset memory care costs in West Virginia, including state Medicaid programs and waivers, Veterans Affairs benefits, private long-term care insurance, and personal/private-pay strategies. Each option has different eligibility rules, covered services, and application processes, so families should use a checklist approach to determine which combos might apply. Below we summarize principal programs and include a compact EAV table to clarify typical coverage and limits. Understanding these options early increases the likelihood of aligning benefits with care needs.
ProgramWhat It CoversTypical Limits / NotesWV Medicaid (waivers)Care services, some in-home or community supports (may exclude room & board)Waivers like ADW can cover services but often require separate room & board paymentVA Benefits (Aid & Attendance)Monthly pension supplements that can be used toward care costsEligibility depends on service history and financial documentationLong-Term Care InsurancePolicy-defined benefits for personal care and facility staysDepends on policy triggers, elimination periods, and benefit caps
How Does Medicaid Support Memory Care Costs in West Virginia?
Medicaid supports memory care primarily through waiver programs that fund home-and-community-based services and certain facility-based supports, though room and board costs are typically not covered by the waiver. Eligibility depends on medical need and financial thresholds, and waivers can provide funding for personal care, some therapies, and case management that reduce out-of-pocket expenses. Families should document medical assessments and financial statements when applying, and expect state DHHR coordination and possible waiting lists for waiver enrollment. Working with an experienced facility social worker or case manager can smooth the application process and clarify what Medicaid will and will not pay.
Memory Care Reduces Nursing Home Admissions for Dementia Patients
Memory care reduces nursing home admissions among assisted‐living residents with dementia
Memory care reduces nursing home admissions among assisted‐living residents with dementia, W Zhang, 2022
What Veterans Benefits Help Pay for Dementia and Memory Care in WV?
Veterans and surviving spouses may qualify for Aid and Attendance and related VA pension benefits that provide monthly supplements useful for paying long-term care costs, including memory care. Eligibility requires proof of military service, financial documentation, and medical evidence of need for assistance with daily living activities. Applications can be complex and often require thorough documentation and possibly professional assistance to optimize the claim. Families should gather service records and medical documentation early and consider seeking help from VA-accredited representatives to navigate the process efficiently.
How Can Long-Term Care Insurance Cover Memory Care Expenses in West Virginia?
Long-term care (LTC) insurance can pay for memory care when the policy’s benefit triggers are met, which usually require documented impairment in activities of daily living or cognitive decline. Policies vary in elimination periods, daily benefit limits, inflation protection features, and maximum benefit periods, so reviewing policy language carefully is essential before assuming coverage. When filing a claim, provide thorough clinical documentation of need and confirm which services and settings the insurer recognizes for reimbursement. If a policy exists, contact the insurer early and request a benefits review to estimate likely coverage for memory care.
What Private Pay and Savings Strategies Help Families Afford Memory Care?
Private-pay strategies include using savings, selling or renting property, annuitizing assets, pooling family resources, or tapping retirement accounts to cover memory care while pursuing public benefits in parallel. Short-term options like respite care or adult day programs can bridge gaps while longer-term planning occurs, and some families use structured asset-shift strategies under legal advice to qualify for programs. Because financial planning around long-term care can have tax and eligibility consequences, consulting an elder-law attorney or financial advisor helps families make informed, legally compliant choices. Combining private-pay strategies with benefit applications often provides the most practical path to placement.
Common private-pay approaches families use:
Liquidating non-essential assets to free funds for immediate care.
Using annuities or life insurance conversions to create steady income streams.
Pooling family support to share costs temporarily while benefits are pursued.
Why Is Memory Care More Expensive Than Other Senior Care Options in West Virginia?
Memory care demands higher ongoing expense because it integrates specialized staffing, environmental safety features, and dementia-centered programming designed to maintain function and reduce incidents. This section explains the concrete service features and staffing structures that create higher operating costs, and it examines how purpose-built facilities justify premium pricing through improved outcomes. Recognizing cost drivers clarifies why some facilities charge more and helps families assess value rather than price alone.
What Specialized Services and Staffing Increase Memory Care Costs?
The primary cost drivers are higher staff-to-resident ratios, staff training in dementia care, continuous clinical oversight, and individualized therapeutic programming. Roles such as RNs, LPNs, licensed social workers, and activity coordinators require training and staffing schedules that exceed those in standard assisted living, and 24/7 supervision adds wage and scheduling complexity. Clinical documentation, medication management, and behavior-support plans also demand professional time and record-keeping. These combined services explain why memory care carries a consistent pricing premium compared with non-specialized senior living options.
How Does a Purpose-Built Memory Care Facility Like Braley Care Homes Add Value?
A purpose-built memory care facility focuses design and services specifically on dementia safety and quality of life, offering secure wandering areas, unobstructed nurse sightlines, and a home-like environment that reduces agitation and supports routines. Braley Care Homes Inc., noted as West Virginia’s only dedicated Alzheimer’s, dementia, and memory care facility, emphasizes these design and staffing elements alongside experienced clinical leadership to improve resident safety and daily functioning. The value of purpose-built design shows up in reduced falls, better staff responsiveness, and programming tailored to memory needs, and those benefits help families justify higher monthly costs when prioritizing safety and specialized care.
What Are the Hidden or Additional Costs Families Should Know About?
Families should anticipate potential add-on fees such as move-in or community fees, charges for higher levels of care when needs escalate, specialized medical supplies, extra therapies, and personal items not included in base rates. Additional fees can also arise for transportation, outpatient therapy, or non-covered behavioral supports, so requesting an itemized fee schedule during any tour or assessment is critical. Asking facilities for example invoices or three-month cost projections for different care scenarios helps families avoid surprises. Transparent pricing conversations with facilities reduce disputes later and clarify what services will be billed separately.
Items commonly billed separately:
Higher-level clinical care or one-on-one supervision when a resident’s needs intensify.
Specialized therapies or equipment not included in base monthly fees.
Move-in or community administrative fees charged at admission.
Asking for an itemized fee schedule during assessments helps families anticipate and budget for these additional costs.
How Can Families Navigate Medicaid Eligibility and Application for Memory Care in West Virginia?
Navigating Medicaid eligibility for memory care requires understanding income and asset rules, waiver availability, the application process, and common strategic approaches that preserve benefits while meeting care needs. This section provides a stepwise framework for families to prepare documentation, apply to WV programs, and consult professionals when complex financial situations arise. Clear steps reduce delays and increase the likelihood of timely benefit approval.
What Are the Income and Asset Limits for WV Medicaid Memory Care Coverage?
Income and asset limits change periodically and vary by program, so families should verify current thresholds with WV DHHR before applying; however, eligibility typically hinges on proving financial need plus medical necessity for long-term services. Spousal impoverishment protections may allow a community spouse to retain a portion of income and resources while the institutionalized spouse receives coverage. Because specific dollar limits fluctuate with policy updates, families should gather recent bank statements, tax records, and proof of income to expedite review and rely on state sources for current cutoffs.
What Medicaid Waivers and Programs Support Memory Care in WV?
West Virginia administers waiver programs that can fund personal care, home- and community-based supports, and specific services for older adults with disabilities; programs such as the Aged and Disabled Waiver (ADW) provide targeted services but often exclude room and board. Waivers vary in scope and availability, and some require application and clinical assessment to determine medical necessity. Families should list potential waivers, document clinical need, and work with a facility social worker or case manager to submit supporting materials that match waiver criteria.
How Do Families Apply for Medicaid for Memory Care in West Virginia?
Application steps generally include collecting financial records, obtaining medical documentation of care needs, completing state Medicaid application forms, and submitting waiver assessments when applicable; timelines vary but early preparation helps avoid gaps in coverage. Families should contact WV DHHR to start an application, prepare documentation (IDs, bank statements, medical records), and keep copies of all submissions. Working with an elder-law attorney, certified case manager, or facility social worker can reduce errors and shorten processing times, and it helps families track appeal options if initial determinations are delayed.
What Strategies Maximize Medicaid Benefits for Memory Care?
Common strategies to optimize Medicaid eligibility include documenting medical necessity clearly, using spousal protections where available, and seeking counsel from elder-law professionals for complex asset situations; informal transfers or rushed asset moves can jeopardize eligibility. Consulting professionals early helps families explore spend-down options, permissible transfers, and structured financial tools that comply with program rules. Because individual circumstances differ, families should treat these strategies as planning options rather than legal advice and engage qualified advisers to implement them safely.
What Should Families Expect from Braley Care Homes Regarding Memory Care Costs and Services?
Braley Care Homes Inc. is presented as West Virginia’s only dedicated Alzheimer’s, dementia, and memory care facility and positions itself as a resource for families seeking specialized, purpose-built memory care with clinically experienced leadership. Families should expect Braley to emphasize a secure, home-like environment with design features that support wandering safety and unobstructed nurse sightlines, a staff mix that includes clinically trained professionals, and dementia-focused activities and care processes. The facility offers free assessments to help families understand individualized needs and obtain personalized quotes, allowing clearer cost planning and placement decisions.
How Does Braley Care Homes Ensure Transparent and Affordable Pricing?
Braley Care Homes provides free assessments that result in personalized quotes and an itemized breakdown of services so families can compare options across facilities more accurately. During assessments, staff review clinical needs, daily routines, medication management, and any behavioral supports to determine the care package that matches the resident, and they explain which elements are included versus billed separately. Families are encouraged to request written fee schedules and example invoices to avoid surprises, and to compare those schedules during tours. Transparent pricing conversations reduce confusion and help families plan budgets effectively.
What Specialized Memory Care Services Does Braley Care Homes Provide?
Braley’s core services include 24/7 supervision by trained staff, assistance with activities of daily living (ADLs), medication administration, individualized daily activities and therapeutic programming, and secure wandering areas designed specifically for memory-impaired residents. The facility highlights a home-like environment combined with experienced clinical leadership to tailor care plans for people living with Alzheimer’s and other dementias. These services aim to maintain routine, reduce distress, and preserve functional ability, improving quality of life for residents and peace of mind for families.
How Can Families Schedule a Free Assessment or Tour at Braley Care Homes?
Families interested in a free clinical assessment or a guided tour should prepare basic medical and medication records and a short summary of day-to-day care needs to make the visit most productive. During the assessment, clinical staff conduct a structured interview, observe functional needs, and discuss likely service levels and a personalized pricing estimate so families understand the financial and clinical implications. After assessment, Braley’s team outlines next steps for placement inquiries and coordinates follow-up conversations about timing and any required documentation. A clear assessment helps families decide whether the facility’s care model aligns with the resident’s needs and budget.
What Are the Most Common Questions About Memory Care Costs in West Virginia?
What Is the Average Cost of Memory Care in West Virginia?
Average memory care costs in West Virginia in 2025 typically fall roughly between $3,325 and $5,500 per month depending on city and level of resident need, with local variance driven by staffing, facility design, and services included. Refer to the city table earlier in this article for localized ranges and use facility assessments to convert these ranges into precise quotes for your loved one.
Does Medicare Cover Memory Care Expenses in WV?
Medicare generally does not cover long-term custodial memory care; it may pay for short-term skilled nursing or rehabilitative stays following hospitalization but not for ongoing dementia supervision or room and board. Families should explore Medicaid waivers, VA benefits, and LTC insurance to cover sustained memory care needs.
Are There Financial Assistance Programs for Memory Care in West Virginia?
Yes—primary programs include Medicaid waivers such as ADW, VA pension benefits like Aid and Attendance, and potentially long-term care insurance benefits depending on policy terms; each program has different coverage scopes and application procedures. Families should gather documentation and consult facility case managers or professional advisors to pursue applicable benefits.
How Do Memory Care Costs Vary by Location Within West Virginia?
Costs vary by city due to differences in labor markets, facility supply, and demand concentration; metropolitan centers and areas with purpose-built memory care communities typically show higher average prices than smaller towns. Use local comparisons to judge whether travel for placement or out-of-area options makes financial and clinical sense.
What Are the Benefits of Early Memory Care Planning for Alzheimer's Patients?
Early planning secures better placement choices, allows financial strategies to be put in place, reduces crisis-driven decisions, and improves continuity of care through thoughtful matches between resident needs and facility services. Scheduling an early assessment helps families clarify timing, expected costs, and the level of care likely to be required.
Quick action items for early planning:
Schedule a clinical assessment to map expected needs and costs.
Gather financial documents to prepare for benefit applications.
Visit purpose-built facilities to compare programming and safety features.
How Are Memory Care Costs Projected to Change in West Virginia Over the Next Years?
Memory care costs are influenced by inflation in labor and supply costs and by rising prevalence of Alzheimer’s disease, both of which are expected to sustain upward pressure on pricing over coming years. Recent trends show wage growth for healthcare workers and increased demand for dementia-specific beds, which together push operators to raise fees to maintain staffing and program quality. Families and planners should monitor authoritative sources annually for updated cost and prevalence data and plan for gradual increases when budgeting for long-term care.
What Recent Inflation Trends Affect Memory Care Pricing in WV?
Inflationary pressures on wages, utilities, and medical supplies have increased operating costs for senior care providers, translating into steady annual price adjustments for care services. Wage pressure is often the largest component because memory care relies on skilled, often licensed, staff working in shifts around the clock. Families should expect incremental increases and plan accordingly to avoid funding shortfalls.
How Will Alzheimer's Disease Prevalence Impact Future Memory Care Demand and Costs?
Rising prevalence of Alzheimer’s and related dementias increases demand for memory-capable beds and programs, creating capacity constraints that can elevate prices and lengthen waitlists for specialized facilities. As demand outpaces available purpose-built capacity, premium pricing for quality, secure settings is likely to persist. Expanding capacity and workforce training are long-term solutions, but in the short term families will need to plan for constrained supply.
What Resources Provide Updated Cost and Care Data for West Virginia Families?
Families should consult national and state-level sources that publish annual cost surveys and prevalence projections to stay current on pricing and demand trends; regular reference resources include national cost surveys, Alzheimer’s prevalence reports, and state DHHR guidance. Checking these resources annually helps families update budgets, evaluate benefit eligibility, and time placement decisions more effectively.
This guide has presented WV-focused cost ranges, funding options, practical application steps, and facility-level expectations to help families navigate memory care decisions with greater clarity and confidence.
Frequently Asked Questions
What should families consider when choosing a memory care facility in West Virginia?
When selecting a memory care facility, families should evaluate several key factors, including the facility's staff-to-resident ratio, the qualifications and training of caregivers, and the types of programs offered. It's also important to assess the safety features of the environment, such as secure wandering areas and unobstructed sightlines for staff. Additionally, families should inquire about the facility's approach to individualized care plans, the availability of therapeutic activities, and the overall atmosphere to ensure it aligns with their loved one's needs and preferences.
How can families prepare for a financial assessment when considering memory care?
Preparing for a financial assessment involves gathering essential documents such as income statements, tax returns, and any existing insurance policies. Families should also compile a list of assets, including property and savings, to provide a comprehensive overview of their financial situation. Understanding potential funding sources, such as Medicaid or VA benefits, can also be beneficial. This preparation will help families engage in informed discussions with facility representatives and financial advisors, ensuring they explore all available options for covering memory care costs.
What role do family members play in the care of a loved one in memory care?
Family members play a crucial role in the care of a loved one in memory care by providing emotional support, participating in care planning, and maintaining open communication with facility staff. They can help ensure that the resident's preferences and needs are understood and met. Regular visits can also help family members stay informed about their loved one's progress and any changes in care requirements. Additionally, families can engage in activities with residents, fostering connections and enhancing the overall quality of life for their loved ones.
What are the signs that a loved one may need memory care?
Signs that a loved one may need memory care include noticeable memory loss, confusion about time or place, difficulty with daily activities, and changes in mood or behavior. Other indicators may include wandering, difficulty recognizing familiar faces, and challenges in managing personal hygiene or medication. If these signs become apparent, it may be time to consider memory care options that provide specialized support and a safe environment tailored to individuals with cognitive impairments.
How can families ensure quality care in a memory care facility?
To ensure quality care in a memory care facility, families should conduct thorough research, including facility tours and staff interviews. Asking about staff training, resident-to-staff ratios, and the types of activities offered can provide insight into the quality of care. Regular communication with staff and participation in care planning meetings can help families stay informed about their loved one's needs. Additionally, families should observe their loved one's interactions and overall well-being to assess the effectiveness of the care being provided.
What should families know about transitioning a loved one into memory care?
Transitioning a loved one into memory care can be challenging, and families should prepare for emotional responses from both the resident and themselves. It's important to communicate openly about the reasons for the move and to involve the loved one in the process as much as possible. Familiarizing them with the new environment through visits can ease anxiety. Establishing a routine and maintaining regular contact can help the resident adjust. Families should also be patient and supportive during this transition, as it may take time for their loved one to adapt.

Our clinic largest private mental health partnership, with a carefully selected nationwide team of Psychiatrists.
KEEP IN TOUCH.
CONTACT US
Location:
Braley Care Homes
6192 US 60
Hurricane, WV 25526
Phone Numbers:
Referrals and Inquiries: (304) 767-4033
Facility Phone: (304) 201-3677
Facility Fax: (304) 201-3678
AREAS WE SERVE
BUSINESS HOURS
Monday
9:00am – 6:30pm
Tuesday
9:00am – 6:30pm
Wednesday
9:00am – 6:30pm
Thursday
9:00am – 6:30pm
Friday
9:00am – 6:30pm
CONTACT US
Location:
Braley Care Homes
6192 US-60
Hurricane, WV 25526
Phone Numbers:
Referrals and Inquiries: (304) 767-4033
Facility Phone: (304) 201-3677
Facility Fax: (304) 201-3678
AREAS WE SERVE
BUSINESS HOURS
Monday
9:00am – 6:30pm
Tuesday
9:00am – 6:30pm
Wednesday
9:00am – 6:30pm
Thursday
9:00am – 6:30pm
Friday
9:00am – 6:30pm




